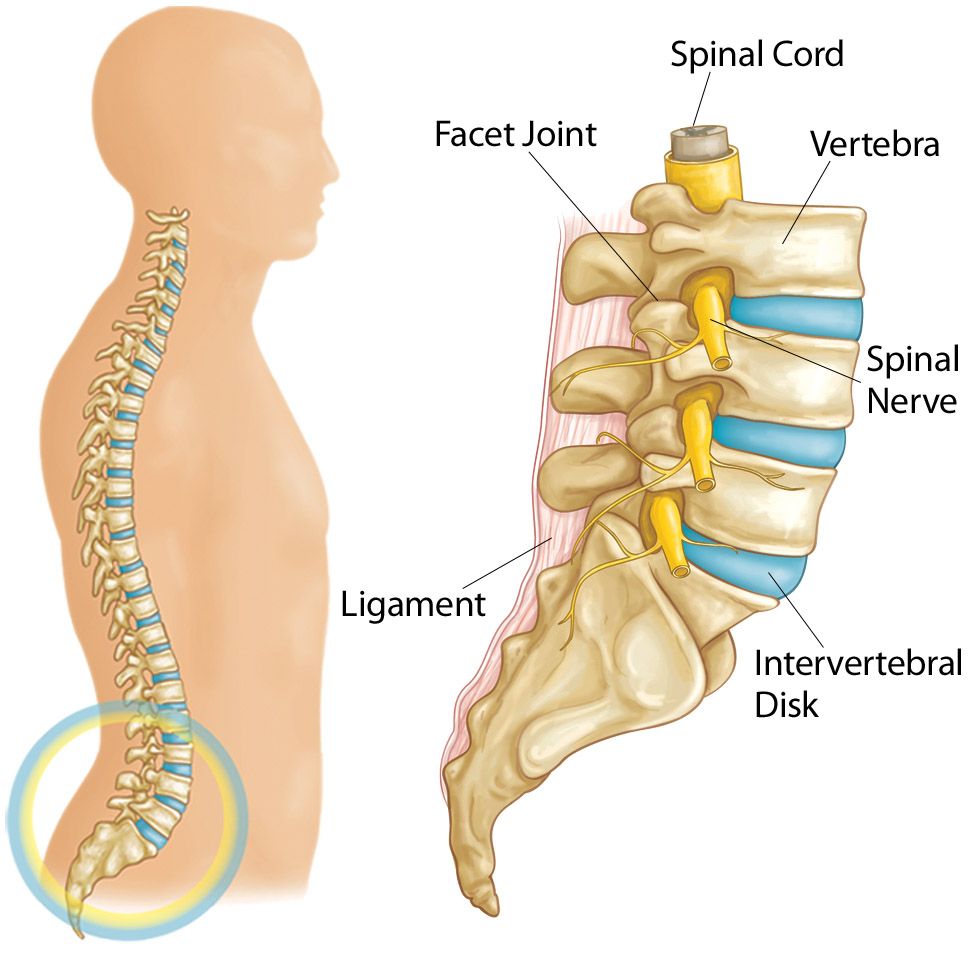
Low back pain can originate from different parts of the spine. In order to fix your low back pain, it is helpful to understand the anatomy of the spine. The bony parts of your spine are known as vertebrae. The soft discs between each vertebrae are called intervertebral discs. These discs are kind of like jelly donuts, the outside ring is thick. On the other hand, the inner part is gelatinous, which allows our spines to bend and flex in multiple directions.
How does back pain happen?
Injury to the discs can occur several ways. Here, we will discuss some of the most common causes of low back pain. This is by no means an exhaustive list, so make sure you consult with your doctor or your physical therapist at Atlantic Physical Therapy for more information about your specific condition.
Sometimes too much force through the spine (often from repetitive lifting or trauma) can cause the gelatinous part to break through the back of the disc. When this happens, the disc can hit the nerves that pass through the spaces between the vertebrae. This often causes burning and tingling pain in the hips, legs or calves. Pain is often worsened with stooping over, slouching, or bending forward.
Another way that the intervertebral discs can become injured is simply wear and tear over time. This is a common part of the aging process. The discs lose moisture and height, which can cause a posterior bulging of the discs. Sometimes when this happens, the nerve roots can also get pinched, causing pain in the low back and sometimes radiation of symptoms in the hips and legs.
Another frequent cause of low back pain is irritation and inflammation of the facet joints. The facet joints are the back part of the bony vertebrae. They compress together when the low back is extended or bending backward. When the low back is extended and the facet joints are pressing together, the space where the spinal nerve roots exit the spine narrows. If there is inflammation in the facets or degeneration of the surfaces of the facets, soreness and nagging pain across the low back is felt with occasional radiation into the hips. Facet joint pain often occurs with prolonged walking or getting up from a chair-the times when the low back is most extended.
The KEY to Fixing Back Pain
The key to fixing back pain is understanding which motions make symptoms worse and which motions improve symptoms. During a physical therapy exam, the therapist will ask you to move into different positions, including, but not limited to, bending forward, backward and side to side. This give the therapist insight as to which motions improve your pain and which motions make your pain worse. Additionally, assessing strength, flexibility, and medical history, gives the therapist vital clues about which exercises and stretches can help decrease your pain.
Give this a try yourself. Start by bending forward as if you were going to touch your toes. Repeat this several times. Pay attention if the motion improves your symptoms, worsens your symptoms, or does not change your symptoms. Now do the same with bending backward. Be sure not to bend your knees while you bend so you get a true idea of how this movement affects your back. After trying these forward and backward motions, you should have an idea of which motion makes you feel better or worse. If neither forward bending or backward bending relieve your symptoms, it’s best to consult with your doctor or Atlantic Physical Therapy physical therapist for further evaluation.
If Back Bending Decreases Your Back Pain Symptoms Read This:
If back bending decreases your symptoms in your legs and centralizes your pain to just your low back, the therapist may give you extension based exercises. Here are some examples of the most frequently given exercises given when back extension decreases your symptoms:
Press Ups: Lie on your stomach which your hands slightly in front of your shoulders. Use your arms to press your shoulders away from your hands, allowing your back to arch. Keep your hips on the ground. Hold right before the point of pain for 5 seconds. Lower back down to the ground. Repeat 20 times.
Standing back bends: Stand tall and place your hands on your low back. Extend backwards without bending your knees. Hold for 1-2 seconds and raise back to standing. Repeat 20 times.
Bridges: Lie on your back with your knees bent and feet flat on the ground. Engage your low abdominal muscles by drawing your belly button towards your spine. Maintain abdominal engagement as you lift your butt away from the floor. Hold for 5 seconds. Lower back to the ground slowly. Perform 3 sets of 10 repetitions.
Try these exercises several times per day. Discontinue any exercise if it worsens your symptoms. Also try to avoid the motions that irritate your symptoms, such as forward bending or stooping. Instead, use your knee to bend to the floor or engage your abs and hinge at your waist instead of stoop.
The good news is that exercise is the most effective way to treat back pain. Plus, the above exercises, make sure you maintain a healthy weight. Another good tip is to take a lot of walks to relieve your symptoms. If your symptoms last more than a week, make sure to consult with your doctor or Atlantic Physical Therapy physical therapist for a customized treatment plan.
If Forward Bending Relieves Your Symptoms, Read This:
If forward bending relieves your symptoms, your physical therapist might recommend exercises that decrease the arch in your low back also known as your lumbar lordosis. These are a few of the most effective exercises given by physical therapists if forward flexing your spine relieves your pain:
Posterior Pelvic Tilt: Lie on your back with your knees bent and your feet on the floor. Slowly bring draw your belly button towards your spine and flatten your back against the ground, taking away the natural arch in your spine. Hold for 5-10 seconds and repeat 30 times.
Modified Thomas Stretch: Lie on your back on an elevated surface or bed. Come to the edge of the surface so one leg can fully hang over the edge. Engage your abdominals by drawing your belly button to your spine. Use a strap, belt, rope or towel to bring the hanging leg towards your buttocks. Be careful to make sure that your thigh remains touching the bed and does not lift off. You should feel a stretch in the front of the thigh and hip. Hold for 10 seconds and repeat 10 times. If this causes you any discomfort in your low back, make sure to loosen the stretch, re-engage your abdominals but pressing your back down into the bed and then re try the stretch.
Double Knee to Chest Stretch: Lie on your back and hug your knees in as if you were going to curl up in a ball. Hold here for 10 seconds and repeat 10 times.
With back pain that improves with flexing your spine, it’s important to remember to engage your abdominals with all transitional activities, such as raising to stand from a chair or getting out of bed. Try to draw your low ribs and belly button in as if you were putting on a tight pair of pants. Your abdominal muscles help to create a corset of strength around your spine, which protects and stabilizes your spine.
The good news is that exercise is the most effective way to treat back pain. In addition to the above exercises, make sure you maintain a healthy weight and make sure to keep your abdominal and hip muscles strong with regular cardio exercise such as recumbent biking. If you continue to have symptoms that last more than a week, make sure to consult with your doctor or Atlantic Physical Therapy physical therapist for a customized treatment plan.
The Atlantic Physical Therapy Method
Health History
When you come to Atlantic Physical Therapy, you are comprehensively evaluated by a Doctor of Physical Therapy. During the first session, the therapist reviews the history of your back pain and your past medical history. You will be asked such questions as:
- Is your pain better or worse with certain activities or movements or with certain positions, such as sitting or standing?
- Is your pain more noticeable at certain times of day?
- Is your pain relieved or made worse by resting?
- What medications are you taking and what other medical conditions are you being treated for?
- Have you had any recent stressful events, injuries, incidents, or environmental factors that you believe might have contributed to your condition?
- What activities is pain inhibiting you from participating in?
- Have you had any imaging studies such as an MRI or x-ray?
Full Examination and Goal Setting
Following the medical history review, your physical therapist will perform a detailed examination. The evaluation will assess your strength, flexibility, balance, coordination, posture, and gait. Your physical therapist will use their hands to examine or “palpate” the affected area to determine the mobility of your joints, muscles, and other tissues. The therapist will assess the affect movement has on your pain by observing you bend and squat.
The therapist will work with you to determine your goals. These goals can include:
- Decreasing or eliminating pain.
- Improving strength and flexibility
- Return to functional, athletic and/or leisure activities.
Your physical therapist will develop a customized treatment plan to address your goals. This may include modalities such as:
- Hot packs/cold packs
- Electrical Stimulation
- Traction/Spinal Decompression
- Spinal Manipulation
- The Graston Technique
- Manual Therapy
- Therapeutic Exercises
- Functional Activity Training
- Mindfulness training and Relaxation Techniques
How will each treatment session play out?
Each treatment session of physical therapy will work towards achieving your goals and addressing impairments in pain, swelling, weakness, or limited motion. Your physical therapist will constantly assess your response to each treatment and will make adjustments as needed. Each session is about an hour, but can be longer or shorter depending on your individual needs.
Your physical therapist will educate you on their findings and the treatments plan. This usually includes teaching you a customized exercise program to do at home to supplement the treatment you receive in the clinic. Your therapist will also teach you proper body mechanics with lifting, squatting, and changing positions in order to prevent symptom flare-ups.
Your physical therapist will determine your need for any special equipment such as a brace. if you do need special equipment, your therapist will instruct you in how to wear and care for the equipment.
Your physical therapist will communicate with your physician by sending reports of examination findings and treatment plans. If your therapist finds that may be in need of additional care such as medication or imaging studies, they will refer you to the appropriate medical professional.
Physical therapy empowers you by teaching you strategies and exercises to decrease or eliminate your pain so you can independently manage the condition. When you are discharged from physical therapy, you will be given exercise instructions for the future. If you ever have any questions, your therapist will be available to help you via phone or email.
If you have additional questions or would like to set up an appointment, call us at 215-271-4100 or contact us here.